
As with any type of surgery, there are complications that may occur following a Breast augmentation or Breast Implant Surgery. It’s very important, that when considering breast implant surgery, you discuss these possible complications with your surgeon. Whilst some issues that lead to occurrence of these complications can be beyond the control of you or your surgeon, the risks can be reduced if you choose a skilled and experienced surgeon who prioritises your wellbeing rather than agreeing with everything you ask for (for example large implants that are not right for your frame), even though he knows that this would cause issues for you in the future.
Many times, correct and suitable implant selection based on patient’s height, width of shoulders and hips, chest anatomy, chest measurements and thickness of breast tissue will minimise the risks and complications. Another important factor that will reduce the risks, is to carefully adhere to your surgeon’s pre and post-surgery instructions. Prevention is always better than Cure…
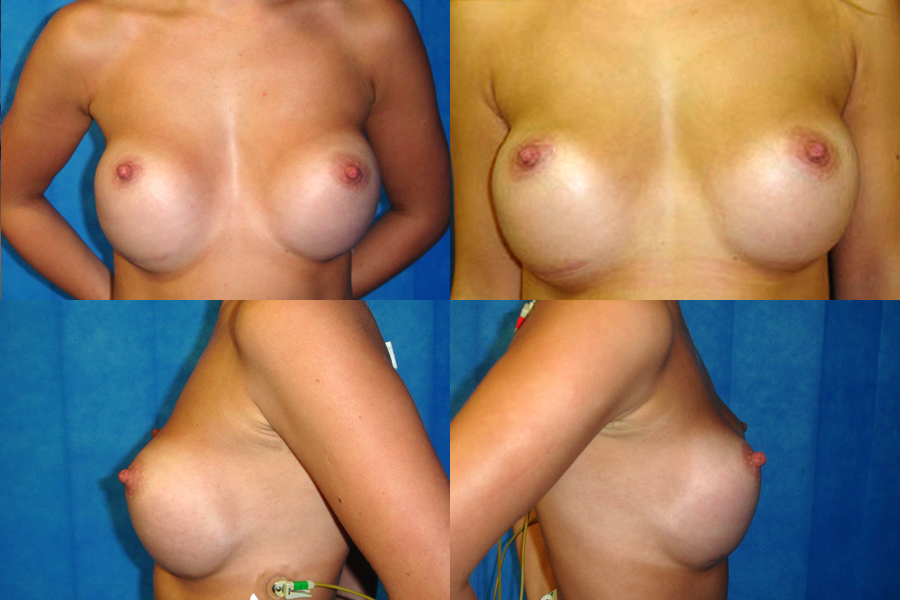
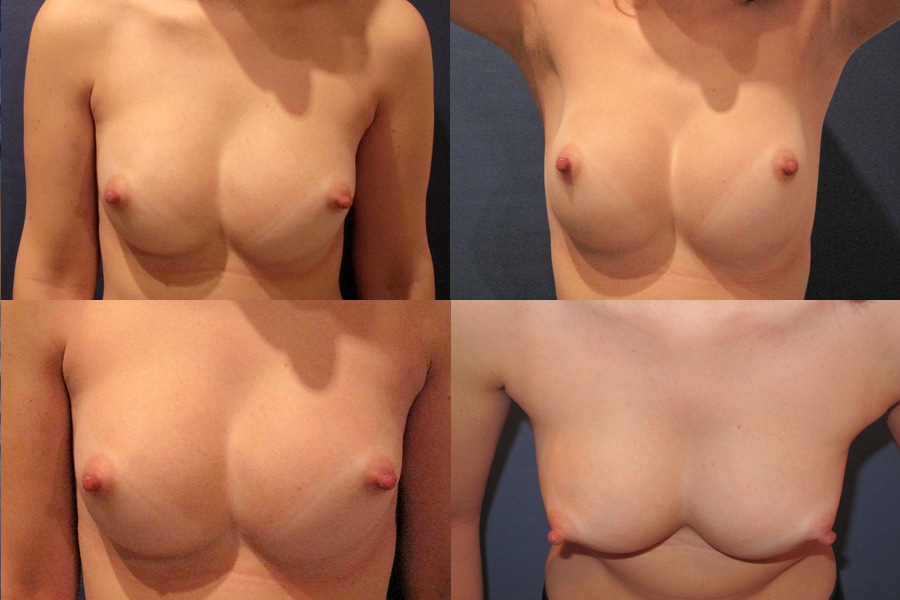
Before & After Photos
To view before and after photos, please refer to the gallery page: Breast Implant Revision Before and After
Here we share with you some of the implant associated complications that although rare, may occur following Breast Implant Surgery.
Wrinkles & rippling

Sometimes following a breast implant surgery, patients may feel and see the wrinkles and rippling of the breast implants under her skin which may feel uncomfortable and gives the breasts an unnatural appearance. Unfortunately, this may be inevitable, especially following pregnancy or significant weight fluctuations as wrinkling and rippling occurs when the breast tissue is stretched, the implant pocket is enlarged and there isn’t enough breast tissue between the implants and the skin.
Particularly prone, are patients with minimal body fat or thin natural breast tissue covering their implants. For these patients, implants (appropriate size) are placed behind the muscle which covers the upper and inner poles of the implant and they will seldom experience any ripples or wrinkles along these areas. They may, however, see and feel the edge of the implants on the lower and outer sides of the breast, as these sides are not covered by the muscle. And unfortunately, nothing can be done in these cases, except for gaining weight and hoping for the fat tissue in the breast to increase.
Implants placed over the muscle (subglandular) may ripple or wrinkle along any side of the implant. Patients who start out with a more generous amount of breast tissue are much less likely to experience wrinkling and rippling However, as the implants do not have the support of the muscle, gravity and weight of implants, will result in faster stretching of skin and breast tissue causing visible wrinkling and rippling on the upper and inner poles of the breast, particularly following pregnancy and weight fluctuations.
It is important to note that the quality of the skin, significantly influences the shape of the breasts and the likelihood of developing wrinkles and rippling. Even though breast skin contains special elastic fibres, there is natural and hereditary variation in the amount of elasticity and thickness of each person’s breast skin, which affects the overall appearance of the breasts.
It is important for patients to know beforehand that they may experience wrinkling and rippling problems following breast implant surgery and what they may do to reduce the risk.
The risks of developing wrinkles and rippling can be significantly reduced if:
- Appropriate implant size is chosen – large implants always increase the risk for wrinkling and rippling.
- Implants are placed in appropriate pocket – i.e. placing the implants submuscular in patient with little to no breast tissue to cover the implant
- Patient maintains same weight following surgery – by losing weight, means also losing breast tissue resulting in the implants coming closer to the skin.
- Complete one’s family prior to undergoing surgery – pregnancy and breast feeding will result in stretching of breast tissue and implant pocket, and many times in significant breast size fluctuations.
Treatment of wrinkles and rippling varies depending on the severity and cause of the condition. In some instances, the condition can be improved by simply gaining some weight, whereas other cases require surgical intervention, involving one or a combination of the following procedures: changing implant size, an uplift or swapping the placement of implants from sub glandular to submuscular.
Mr Rezai will discuss the best treatment options for you, during your consultation.
Leakage & rupture

Breast implants are not life-time devices and need to be replaced at some point in time, regardless of the type or brand of the implants. Some manufacturers state a time limit on the lifespan of their implants, whereas others provide lifetime warranty. None of these statements confirm how long the implants really last. In some patients, implants may rupture within the first few years of the implantation whereas for others their implants may last much longer without experiencing any issues.
When Implants are placed in the breast, the body forms a fibrous tissue, known as “Capsule”, around the implants. When implants rupture, it can be “intracapsular”, meaning that although the shell of the implant is ruptured, the capsule around the implant contains the silicone gel. Many times, this type of rupture can go unnoticed for several years, as there may be no visual or physical symptoms.
However, when the silicone gel does move outside the fibrous capsule, it is referred to as “extracapsular” rupture and this normally alters the contour, shape and size of the breast. In some cases, the gel will gradually migrate away from the breast tissue into the lymph nodes and gather to form a small lump in chest, armpit or arm areas. It should be noted that Silicone-gel ruptures are usually slow acting, meaning the material leaks out over a period of months or years. The extracapsular rupture can normally be detected during a clinical examination whereas to confirm an intracapsular rupture, some type of scan, typically a breast ultrasound, is required.
“Silent Leakage” is a term used when referring to microdroplets of silicone penetrating through the implant shell and the fibrous capsule, despite them being intact. This process can normally take years and the silent leakage becomes apparent when the microdroplets of silicone forms small lump(s) in the breast or the lymph nodes located in the armpit.
Causes of leakage and rupture may include:
- Natural wear and tear
- Punctures following a breast biopsy
- Trauma that may result from an accident or a violent impact against your chest
- Manufacturing fault – small, unavoidable imperfections in the silicone shell of the implant
When an implant ruptures, the most apparent sign is that the breast becomes firm and swollen (doubles in size), remains swollen for about a week then returns to normal size. Other symptoms may include:
- Pain, burning, tingling, numbness, hypersensitivity or redness in the affected breast
- Small lumps in and around the breast, armpit or arm
- Distorted breast shape
- Softening of the breast
- Breast asymmetry
It is important to remove a ruptured implant soon after rupture is confirmed, particularly if it is an extracapsular rupture. Any delays will increase the risk of the silicone migration. However, due to various reasons, patient may not be able to undergo surgery as soon as she’d like to and, in these instances, it is crucial to wear an extra high impact sports bra, day and night, avoid putting any pressure over the chest area and stop any strenuous activity or sports until the ruptured implant have been removed or replaced.
If you suspect your implant has ruptured, although there is no threat of serious health problems, it is important to contact your surgeon or GP as soon as possible to have this confirmed and discuss best course of action.
BIA-ALCL
Breast Implant Associated Anaplastic Large Cell Lymphoma, BIA-ALCL, is an extremely rare and highly treatable type of non-Hodgkin’s lymphoma, a cancer of the cells of the immune system, that can develop around breast implants. It is important to note that even though BIA-ALCL is found in the breasts of some women with breast implants, it is not breast cancer. BIA-ALCL develops in the fluid around breast implant and is usually contained by the fibrous capsule around implants.
To date, no specific causal factors for BIA-ALCL have been identified. However, it does appear that textured implants are associated with more cases of BIA-ALCL than smooth implants.
Common Symptoms include persistent swelling of the breast, tenderness, overlying skin rash and fluid accumulation around the implant. It can also present as a lump in the breast or armpit. For any patient experiencing these or any symptoms, they should see their plastic surgeon for evaluation, testing and diagnosis.
BIA-ALCL is extremely rare and no different to any other implant related complications and is treated with the removal of both breast implants and the tissue capsule around them (total capsulectomy) from both breasts. If patient wishes to re-augment her breasts, this can be done 12 months after the implants and capsules have been removed.
At your consultation with Mr Rezai, you will be provided with detailed information about this rare complication.
For Up-to-date information about BIA-ALCL visit:
Bottoming out
Bottoming out is a complication that occurs when the implant slides too low in the breast tissue, increasing the distance between the nipple and the breast fold causing the nipple to point upwards. Bottoming out is normally caused when:
- There is skin laxity, caused by, natural ageing, weight fluctuations, pregnancy, breast feeding and other hormonal changes impacting the breast tissue.
- The surgeon over dissects the implant pocket, placing the breast fold too low.
In addition to the above, smoking, large implants, high concentration of breast fat and not supporting the breasts while exercising or being active, can also increase the risk for developing Bottoming Out.
Bottoming out can only be corrected surgically. The corrective surgery normally involves re-creating the breast implant pocket and many times combined with an uplift. In some cases, the correction process may be completed in 2 stages:
- Remove the implants, and if necessary, re-adjust/repair the breast pocket and allow the breast tissue to heal over 6-9 months.
- Once breast is settled and healed, re-augment using an appropriate size implant and suitable placement. Sometimes an uplift will also be necessary to remove excess skin.
Double bubble

“Double bubble” occurs when an implant or natural breast tissue drops down below the breast fold (inframammary crease), creating an unnatural indentation or line across the lower pole of the breast; causing the appearance of two breasts, from the profile. This condition is more visible when the arms are lifted above the head. Fortunately, double bubble is a relatively rare complication which may occur at any time after breast augmentation surgery and it is treatable in most cases.
The following scenarios can result in Double Bubble:
Incorrect breast implant placement – Double bubble occurs when a patient that has sagging breast tissue and is indicated for a subglandular implant placement but instead undergoes a submuscular placement. This results in a full upper breast pole but with low hanging breast tissue giving the appearance of a second hanging breast.
Pregnancy – Following pregnancy, the breasts become larger, the natural breast tissue sags, but the implants remain where they were originally placed.
Oversized implants relative to your size– When implants are too big and heavy for the chest wall it causes skin and supporting breast tissue to stretch and settle or migrate below the natural breast fold.
Double bubble may also occur when:
- Patient has tuberous breast deformity
- Ageing causes natural sagging of the natural breast tissue, but the implants remain where they were originally placed.
- Natural breast fold is too high, this means the distance between the nipple and the breast fold is too short and as a result, a new lower fold is created but there is a visible groove between the nipple and the new lower fold.
- Patient develops capsular contracture – scar tissue build-up and hardening of the fibrous capsule surrounding the implant
- Scarring is present from previous breast surgeries
It should be noted that Double Bubble is rare and many patients with similar scenarios as above, may not develop this problem.
There are various ways of handling or correcting Double Bubble. Here are some of the treatment options:
- Prevention is better than Cure – it is best to try to avoid developing this complication by choosing a plastic surgeon who is skilled and experience in breast implant surgery and also to listen to his advice and recommendation regarding appropriate implant sizes for your anatomy and frame.
- Sometimes treatment may not be necessary, and the double bubble will resolve on its own. In some cases, your surgeon may advise you to wait for up to a year after your breast augmentation to see if it improves on its own, before making a decision to undergo further surgery to correct it.
- Surgical intervention – this type of correction various depending on the cause of the double bubble. This treatment can involve, one or a combination of the following: a breast uplift (mastopexy), changing size and/or placement of implant and adjusting the breast fold.
The right way of handling / correcting Double Bubble depends on the cause, patient’s current anatomy and how long after surgery this occurs. Your surgeon should discuss the best treatment options for you, during your consultation.
High riding

Following Breast augmentation, implants may appear to be sitting slightly too high and to have too much fullness in the upper half, especially when implants are placed submuscular or dual plane. This is completely normal, and It takes time for the muscle and tissue to relax and allow the implants to settle in place. The healing period and the settling of breast implants, varies between individuals and is determined by their chest anatomy.
However, sometimes the implants are placed too high in the breasts, or patient may develop complications which may result in implants looking unnatural and high on the upper pole of the breast. This condition is known as “high riding” and can only be corrected with surgical intervention.
Individuals who undergo high riding implant revision have one or more of the following problems with their breast implants:
Reasons for High Riding implants may include:
- Inadequate muscle release
- Poor pocket development
- Early capsule formation
- Patient has a strong muscle
- Rough textured implants – Attachment of breast tissue to surface of breast implant.
Surgery to correct High Riding implants and to achieve a more natural looking breasts may involve release of the muscle, increasing the size of the implant pocket, excising the capsule.
Mr Rezai will discuss the best treatment options for you, during your consultation.
Symmastia (Uniboob)
Symmastia also known as “uniboob” or “Monoboob”, is a very rare implant complication that occurs when the skin and muscle between the breasts over the sternum (breastbone) detaches and the two pockets of tissue that hold the breast implants come together to form one pocket. In practical terms, what that means is that the cleavage is not as deep as it should be with the skin along the midline lifted up and creating the appearance of a single large breast.
A number of factors can contribute to the development of Symmastia:
These include:
- Implants that are too large for one’s anatomy.
- Creating an implant pocket that is too big
- Over releasing of the pectoralis muscle from the chest wall in order to create a narrower cleavage.
- Patients with pre-existing chest wall deformities are at higher risk of developing this complication.
- Congenital condition where the individual’s natural anatomy is predisposed to the development of Symmastia. This is especially the case in those who have very loose and mobile skin along the midline and typically these women have their pec muscles inserted close to or at the midline.
It’s often difficult to correct Symmastia and it may require more than one surgery.



















